How else can it be called?
Urethral syndrome
ICD-10: N34
What is urethritis?
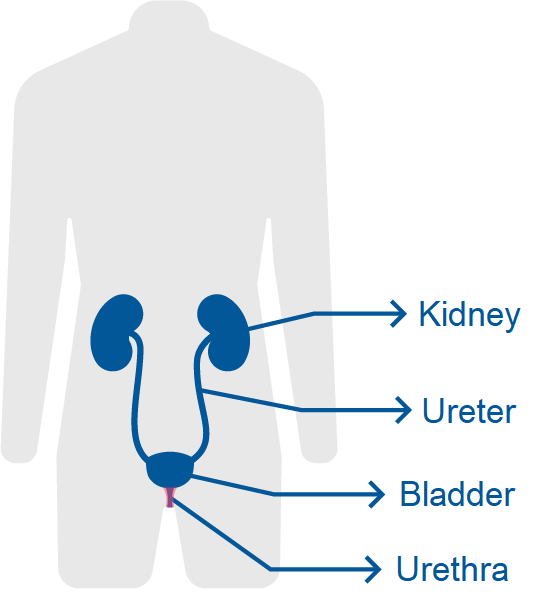
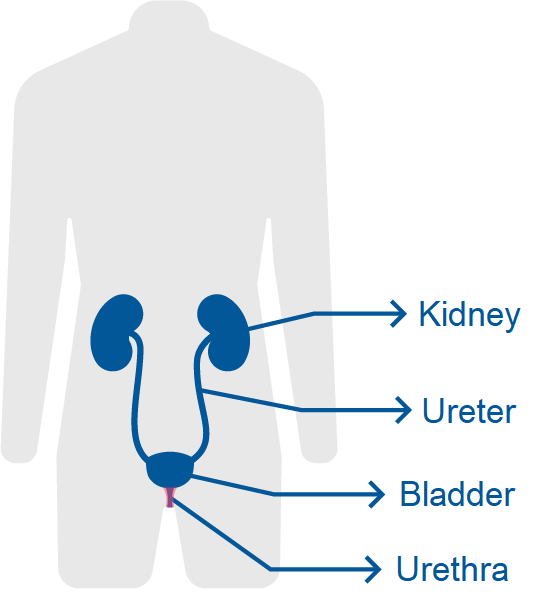
Urethritis refers to the inflammation of the urethra where it becomes irritated and swollen.
The urethra is the thin tube that carries urine from the bladder to the outside of the body.
Urethritis can occur in men and in women and may last for weeks or months.
What are the main causes?
Urethritis can be divided into two main groups depending on the causes:
- Gonococcal urethritis: Caused by the bacteria responsible of gonorrhea (neisseria gonorrheae).
- Non-gonococcal urethritis: Not related with gonorrhea.
- Due to infection by other bacteria or viruses (Chlamydia trachomatis, mycoplasma genitalium, etc.).
- Urethral stricture (narrowing of the urethra caused by injury or structural problems).
Almost all the viruses, bacteria and parasites responsible of STDs (Sexually Transmitted Diseases) can cause urethritis (for example gonorrhea, chlamydia, etc.).
It is called urethral syndrome when symptoms are present but there is no evidence of infection by viruses or bacteria.
What are the main symptoms of urethritis?
The main symptoms of urethritis are:
- Excessive urgency and frequency of urination.
- Dysuria: Pain, discomfort or burning in the urethra and lower abdomen when urinating.
- Urethral discharge that can be bloody (with blood) or purulent (with pus).
How can it be diagnosed?
For a proper diagnosis of the disease the following screening tests are available:
- Urinalysis, that may reveal the presence of an infection
- Urine culture with antibiogram to confirm the infection, to know the virus or bacterium involved and to prescribe the appropriate antibiotic.
- Urethral discharge culture or genital culture to detect any STD (Sexually Transmitted Disease)
- Cystoscopy, to look inside the urethra and bladder using a thin camera. This procedure is not always necessary. It is usually performed when the urethritis cannot be cured or the cause is unknown.
What is the recommended treatment?
Once diagnosed, the treatment requires antibiotics (ceftriaxone, doxycycline, azithromycin) and after the full course of medication, a culture is performed to confirm the efficacy.
When urethritis does not clear up after treatment and last for more than 6 weeks is called chronic urethritis.
Women with recurrent episodes of urethritis or cystitis may be prescribed with a postcoital dose of antiseptic (to be taken shortly before or after sexual intercourse).
People with urethral syndrome (symptoms without evidence of infection) may be treated with phenazopyridine to decrease discomfort with urination.
What is the prognosis of the disease?
In most cases, it is possible to know the causal agent and start the treatment with a good prognosis.
How can it be prevented?
It is advisable to drink much water.
Women with urinary tract infection associated with intercourse (the symptoms appear within 24 hours of intercourse) should urinate right after intercourse.
It is also important to follow good hygienic practices by the affected person and by their partner. Hygiene should be adequate, neither excessive nor deficient. Soaps suitable for the genital area (not excessively aggressive) are the appropriate ones.
Safer sex practices may reduce the risk of transmission of STDs (Sexually Transmitted Diseases) related to urethritis.
As soon as the first symptoms appear, it is important to follow a proper care in order to avoid a persistent damage to the tissues.
Which are the main complications of urethritis?
Urethritis infections may have long-term consequences when left untreated, such as pyelonephritis (kidney infection) or a structural damage to the urinary tract.
Bibliography
- The Diagnosis and Treatment of Male Infertility: A Case-Based Guide for Clinicians, Nabil Aziz and Ashok Agarwal, ISBN 978-3-319-56545-3, Chap. 6.
- Robbins Basic Pathology (10th Ed) 2018, Vinay Kumar, Abul K. Abbas, Jon C. Aster, ISBN: 978-0-323-35317-5, Pag. 709.
- Diagnostic Pathology of Infectious Disease. 2nd edition. Richard L. Kradin. 2018. ISBN: 978-0-323-44585-6. Pág. 429.
- Sexually Transmitted Infections in HIV Infected Adults and Special Populations, Laura Hinkle Bachmann. 2017. Pag 9. ISBN: 978-3-319-56692-4.
- European Association of Urology Guidelines on Urological Infections: Summary of the 2024 Guidelines. Kranz, Jennifer et al. En: European Urology, Volume 86, Issue 1, 27 - 4. Julio 2024. 3.9 Urethritis. Available on: https://www.europeanurology.com
- Sexually Transmitted Infections Treatment Guidelines, 2021. En: Centers for Disease Control and Prevention - Morbidity and Mortality Weekly Report MMWR - Recommendations and Reports / Vol. 70 / No. 4 - July 23, 2021. Diseases Characterized by Urethritis and Cervicitis. Págs. 60 - 80. Available on: https://www.cdc.gov
Show more
Rating Overview
Share your thoughts about this content