How else can it be called?
Upper urinary tract infection
ICD-10: N12
What is pyelonephritis?
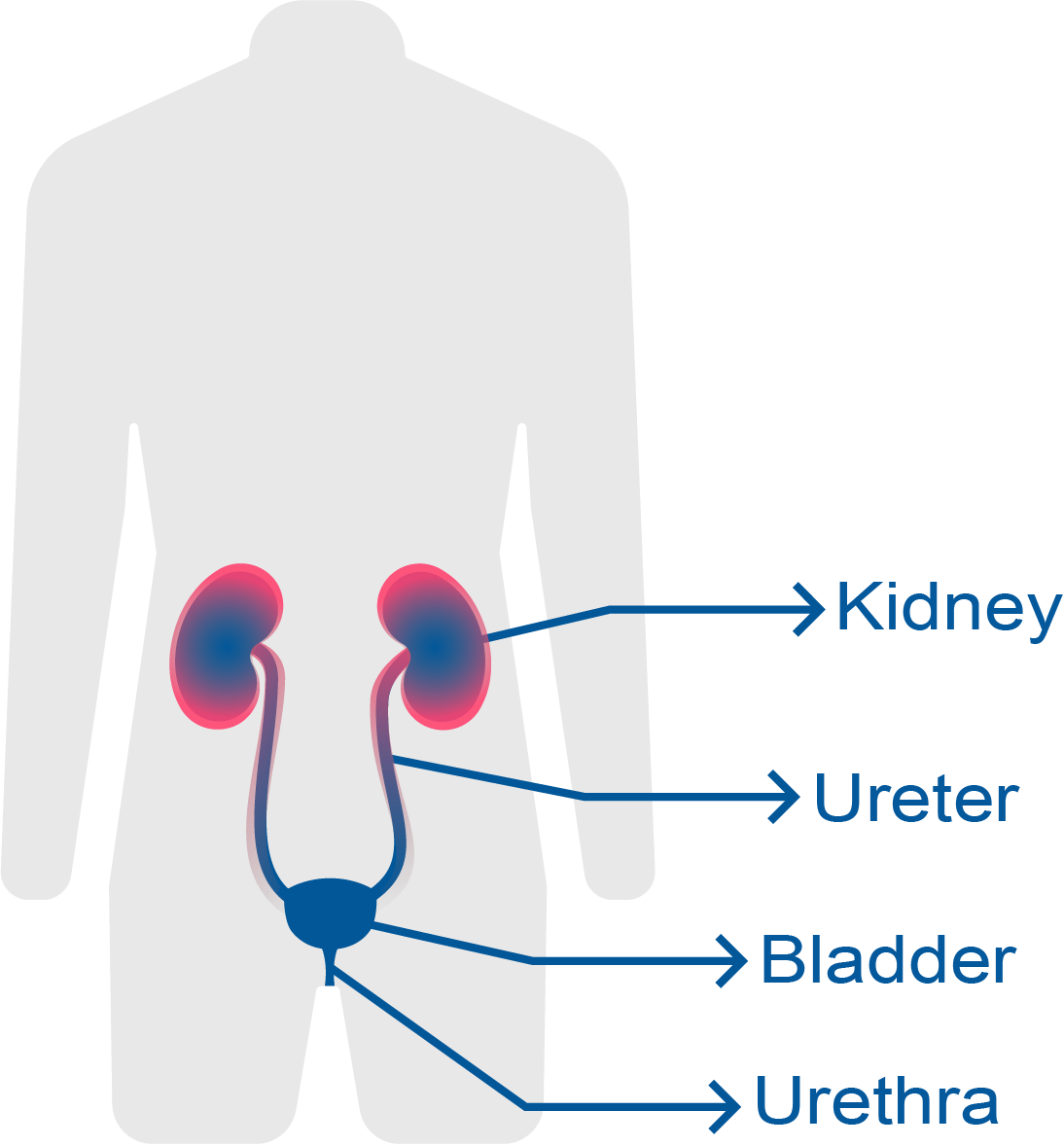
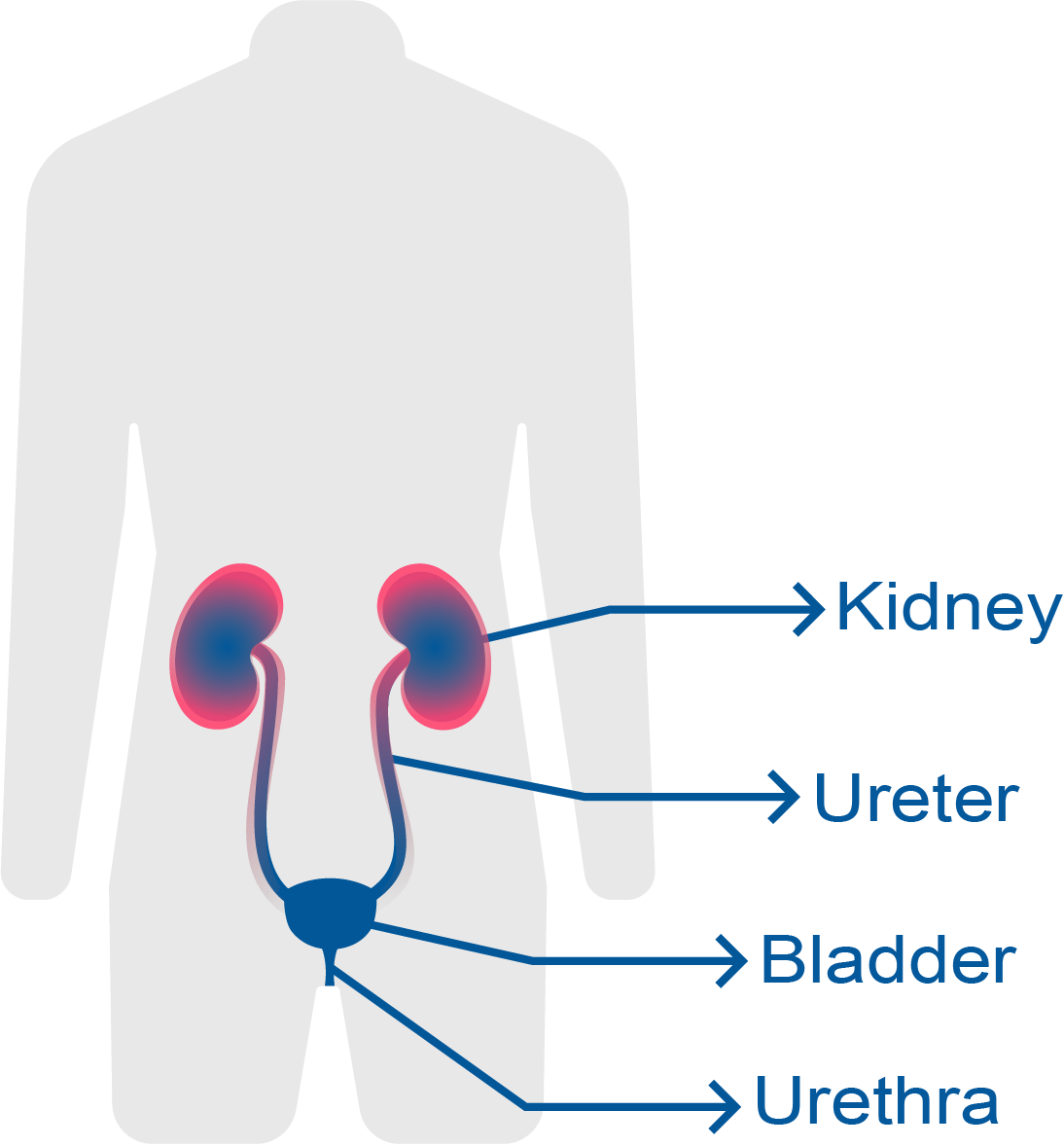
Pyelonephritis is an inflammation of the kidney and upper urinary tract that usually results from bacterial infection.
Pyelonephritis is also called upper UTI (urinary tract infection) because it affects, in addition to the kidneys, the ureters that carry urine from the kidneys to the bladder.
Common bacterial causes include Escherichia Coli and Enterococci species.
Which are the different types of pyelonephritis?
Pyelonephritis can be classified into:.
- Acute pyelonephritis: Acute pyelonephritis most frequently occurs as a result of ascending movement of bacteria from a lower UTI (a cystitis for example). It is a more serious infection than a cystitis but it is usually well managed with the proper treatment. It can be a serious condition in elderly or immunocompromised people (for example, people with cancer or VIH).
- Chronic pyelonephritis: It is a more serious infection often due to congenital urinary structural defects. The main possible complications are sepsis (overreaction to an infection) and kidney failure (the kidneys cannot filter waste product from the blood).
Pyelonephritis usually happens associated with vesicoureteral reflux where urine flows backward from the bladder. In these cases, there are usually recurrent acute pyelonephritis or chronic pyelonephritis.
What incidence does it have?
Women are infected five times more often than men with an estimated annual incidence of 120 to 130 cases per 100.000 women and 30 to 40 cases per 100.000 men.
What are the main symptoms of pyelonephritis?
The main symptoms of pyelonephritis are:
- Fatigue and weakness
- A fever greater than 102°F (39°C) for two or more days
- Chills
- Flank pain (aching pain on one or both sides of the lower back)
- Abdominal pain (sometimes)
- Nausea and vomiting
- Pain or burning with urination (dysuria)
- Frequent urination, nocturnal urination, etc.
- Cloudy urine
- Bloody urine
- Foul smelling urine
How can it be diagnosed?
The common tests and procedures used for the diagnosis are:
- Physical exam: Tenderness to palpation in the kidney region.
- Urine test: The urine tests will show the presence of white blood cells, red blood cells, proteins and urinary casts.
- Urine culture: Urine cultures will show bacteria in the urine. They are usually bacteria of the gram-negative family.
- Abdominal ultrasonography: A noninvasive procedure that may show signs of pyelonephritis.
- Intravenous urography: X-ray procedure that uses an injection of contrast material to evaluate the kidneys and ureters. In pyelonephritis it will show diffuse low-attenuation change. In addition, it may detect diseases that cause a chronic or recurrent pyelonephritis.
What is the recommended treatment?
The ultimate goal of acute pyelonephritis treatment is the control and remission of the infection. In addition, the treatment tries to reduce acute symptoms that usually persist more than 48 hours after the start of treatment.
The most common treatments used are:
- Antibiotics: They are used to fight against the bacterial infection. The most used ones are antibiotics such as TMP/SMX (Trimethoprim/sulfamethoxazole) and ciprofloxacin. If the infection is severe or the risk of complications is high, they must be given by an intravenous (IV) injection. Antibiotics may be required for a long time.
- Analgesics- antipyretics: Drugs to fight against pain, fever and weakness.
- Intravenous fluids: To prevent dehydration and ensure that medication reach the kidneys quickly.
Chronic pyelonephritis may require high doses of antibiotics for as long as six months to clear the infection. Surgery is sometimes necessary if the patient has complications caused by obstructions, or to eradicate infection.
The treatment of any complication should be precise and effective. It may include hospitalization in an intensive care unit, cardiac monitoring and any other treatment. The underlying causes must be treated.
Urine cultures are repeated as part of the follow-up of patients with chronic pyelonephritis to ensure that bacterial infection is completely cleared.
Which are the associated complications and risks?
The risk of complications is increased in case of:
- Vesicoureteral reflux: The urine flows backward from the bladder, up the ureter to the kidney. There may be urine retention in the renal pelvis (the enlarged upper end of ureter in the kidney).
- Obstructive uropathy: The flow of urine is blocked. There are multiple causes for obstructive uropathy such as pregnancy, abdominal mass, etc. The most common cause is urolithiasis (kidney stones or urinary calculi).
What is the prognosis of pyelonephritis?
The prognosis for most patients with pyelonephritis is quite good if the infection is caught early and treated promptly. Sometimes the treatment may be long and aggressive. In any case, the treatment must avoid complications such as:
- Recurrences
- Sepsis (severe response to infection)
- Kidney failure (kidneys do not work properly)
How can it be prevented?
The treatment of cystitis, bladder infections and other UTI (urinary tract infections) may prevent in many cases the development of pyelonephritis.
In addition, it is necessary the prevention of conditions that increase the risk, such as vesicoureteral reflux and obstructive uropathy.
Bibliography
- First Aid for the Basic Sciences: Organ Systems (3rd Ed) 2017, Tao Le, William L. Hwang, Vinayak Muralidhar, Jared A. White and M. Scott Moore, ISBN: 978-1-25-958704-7, Pag. 638.
- Diagnostic Pathology of Infectious Disease. 2nd edition. Richard L. Kradin. 2018. ISBN: 978-0-323-44585-6. Pág. 429.
- Bacterial Infections and the Kidney. Anjali A. Satoskar, Tibor Nadasdy. 2017. Pag 161. ISBN 978-3-319-52790-1.
- The Gale Encyclopedia of medicine. Second Edition. Jacqueline L. Longe. Vol 4. pag 2789. ISBN 0-7876-5493-0.
Show more
Rating Overview
Share your thoughts about this content