


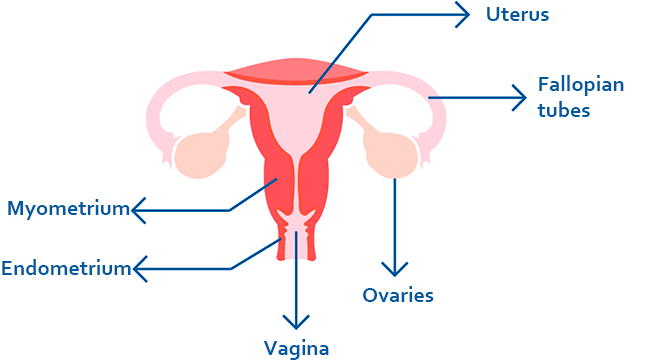
Pelvic inflammatory disease describes an infection of the female reproductive organs which includes the uterus, ovaries, Fallopian tubes and, pelvic tissues.
It is a very common disease, difficult to diagnose and with serious consequences if no treatment is prescribed.
Pelvic inflammatory disease is usually caused by microorganism, most time transmitted by a sexual intercourse.
It may be caused by intestinal infections or other type of infections that spread to the female reproductive organs, but it is rare.
It is developed when the microorganisms move upwards from the cervix to the uterus, Fallopian tubes or pelvic cavity.
The most common microorganism involved are Neisseria gonorrhoeae (gonococcus) and Chlamydia trachomatis. Others microorganism such as Mycoplasma genitalium or anaerobic bacteria can also produce PID, as well as not infectious bacteria normally present in the vagina.
In the pelvic inflammatory disease, the cause is usually a combination of an infection of different types of bacteria at the same time.
Some factors increase the risk for an infection of the female reproductive organs:
Many women are asymptomatic, and they notice the disease only when they want to get pregnant and visit their doctor because they are unable to do it.
Other women have symptoms that range from mild to severe.
The most common symptoms of the acute PID are:
In case of suffering from chronic PID, the symptoms can be:
The pelvic inflammatory disease may be present with acute pelvic pain. If there is an abscess or pus it is then considered an emergency.
There are some signs and tests that may help in the diagnosis such as transvaginal sonography, computed tomography (CT) and lab tests (pregnancy test, WBC count and C-reactive protein level).
If not-urgent, tests for chlamydia, gonorrhea and mycoplasma are performed. In addition, it is advisable to test for a possible HIV infection and syphilis.
Other times, pelvic inflammatory disease may be present with no symptoms or chronic pelvic pain. In these cases, there is no test for an accurate diagnosis and the symptoms can suggest the doctor to prescribe you a treatment to prevent future complications.
Treatment with antibiotics is essential at the beginning of the disease. If it is not treated properly, the disease can lead to complications such as scarring of the Fallopian tubes and other tissues of the of the pelvic cavity, infertility, chronic pelvic pain, pelvic adhesion or pelvic abscess.
In general, it is a treatment with a mixture of antibiotics depending on the bacteria involved and the antibiotic resistance of the geographical area.
If the woman uses an IUD (intrauterine device) it is necessary to remove it.
All the sexual partners from last 60 days of the person infected should be also treated. It is necessary to avoid any sexual intercourse until the infection is solved.
Some herbs of the alternative medicine can be useful such as Echinacea and calendula for their antibacterial activity.
Nutrition also plays an important role to keep the immune system working well. It is recommended to eat fresh vegetables and fruits, restrict the intake of processed food and take supplements of vitamin A, C and B to help the immune system.
The best way to prevent the transmission of the disease is the use of condom in sexual activities.
If you feel acute abdominal pain, with or without fever, you must visit your doctor because it can be a sign of pelvic inflammatory disease that requires immediate attention.
If your menstrual cycles have been regular and become irregular or with heavy bleeding, please ask your doctor.
Important: Pelvic inflammatory disease must be treated as soon as possible to avoid infertility in the future (the most common complication).