How else can it be called?
Heart attack
ST-elevation myocardial infarction
Coronary artery disease type heart attack
ICD-10: I21
ICD-11: BA41
What is a myocardial infarction?
A myocardial infarction, also known as a heart attack, is caused when a part of the heart muscle (the myocardium) starts to die due to a lack of blood flow.
An infarction is an area of a tissue that has died from the lack of oxygen. The myocardium is responsible for contracting and pumping blood throughout the circulatory system.
It is important to understand that a heart attack is a medical emergency that requires immediate attention. If you suspect that you or someone else may be experiencing a heart attack, seek immediate medical attention. Delaying medical care can be life-threatening and results in thousands of deaths every year.
What are the main causes of myocardial infarction?
A heart attack occurs when the heart muscle is unable to receive enough oxygen due to advanced coronary disease.
Certain individuals are at higher risk of experiencing a heart attack:
- Males
- Females after menopause
- Smokers
- People with obesity, diabetes mellitus and high blood pressure
- In case of family history of cardiovascular disease
- When cholesterol levels are high
- In people with a previous coronary disease: angina pectoris, previous myocardial infarction or altered exams
The coronary vessels, which supply oxygen and nutrients to the heart muscle, can develop atheromatous plaques, consisting of fats, calcium, and other substances that compromise the flow of oxygen and nutrients to the heart.
The narrowing of the vessels can result in blood flow problems that range from angina, which is temporary, to a heart attack, which is permanent and irreversible.
The presence of atherosclerosis in a blood vessel can lead to the development of a thrombus, which is a clot of platelets, coagulation proteins, and cellular debris that clogs the vessel.
An embolus is a thrombus that travels through the blood until it lodges in a small vessel, causing an embolism. Therefore, thrombosis and embolism are equivalent terms.
What are the main signs and symptoms of a myocardial infarction?
The following signs and symptoms are common in a myocardial infarction:
- Severe and prolonged chest pain that feels like intense pressure and can radiate to the arms, shoulders (especially the left), back, teeth, and jaw.
- The pain is described as a huge fist twisting the heart. It is similar to that of angina, but longer in duration, and does not respond to nitroglycerin under the tongue.
- The pain sometimes does not follow any fixed pattern and may be perceived differently, especially in women, the elderly and diabetics, where it may be present as prolonged pain in the upper abdomen, which may be attributed to indigestion.
- Difficulty breathing.
- Dizziness (which may be the only symptom in 10% of cases).
- Others: Nausea, vomiting, fainting, and sweating may occur.
- Previous history of unstable angina: frequent attacks of angina pectoris not linked to physical activity.
How can it be diagnosed?
The following methods are commonly used in the diagnosis of a heart attack:
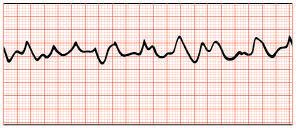
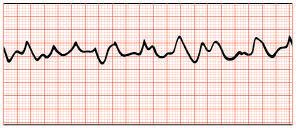
- ECG (electrocardiogram): An ECG is often the first diagnostic test done when a person experiences symptoms of a heart attack. It involves attaching electrodes to the skin to measure the electrical activity of the heart. An ECG can help identify abnormal heart rhythms and changes in the heart muscle that are indicative of a heart attack. If you are admitted to a coronary care unit, you will be monitored with an ECG for the duration of your stay.
- Biochemical Markers of Myocardial Damage: Blood tests that measure levels of certain enzymes and proteins in the blood can help determine if a heart attack has occurred. The most important markers are troponin and CK-MB (creatine kinase isoenzyme MB).
- Nuclear cardiology and/or cardiac catheterization (coronary angiography). These tests are typically done after the acute phase of a heart attack has passed.
After diagnosis, patients are typically observed in the hospital for several days and allowed to gradually increase their activity.
The length of hospital stay can vary but is generally between 7 and 14 days.
What is the prognosis of myocardial infarction?
Survival rates after a heart attack depend on the size of the infarct and the extent of damage to the heart's electrical system. Small infarcts that do not affect the electrical system often have a good prognosis.
However, one in three people die from a heart attack before they can receive medical attention, which is known as sudden death.
Thankfully, improvements in cardiopulmonary resuscitation (CPR), diagnostic tests, and urgent care have led to better survival rates.
Due to the possibility of a sudden death, it's crucial to apply CPR techniques as soon as possible to increase the chances of survival. In fact, most people who survive two hours after a heart attack will survive.
After an acute coronary syndrome, electrocardiographic monitoring is recommended every six months, even if there are no symptoms.
Echocardiograms are also done to assess the recovery of the heart muscle.
To prevent another heart attack, interventions such as angioplasty or coronary bypass surgery may be recommended. Additionally, lifestyle changes like giving up smoking, following a healthy diet, and doing exercise regularly can also help prevent future heart attacks.
Which complications may arise?
Complications can arise after a heart attack, including:
Cardiac arrhythmia
The bio-electrical system controls the heartbeat. A heart attack can damage this system, leading to serious arrhythmias such as ventricular fibrillation. This condition causes the ventricles to contract rapidly and ineffectively, preventing the heart from pumping blood and leading to cardiac arrest.
In some cases, slow heart rhythms known as heart blocks may occur, requiring the implantation of an artificial pacemaker temporarily or permanently.
Heart failure
If the infarct area is extensive, the remaining healthy heart muscle may not be able to compensate for the loss to pump effectively.
Death
In one in four people who suffer sudden death, there were no previous symptoms of heart disease. By far the most common cause of sudden death from a heart attack is ventricular fibrillation.
What is the recommended treatment?
The main recommendations and treatments for a heart attack are:
- Call for help immediately if you experience crushing chest pain that lasts for more than five minutes. Do not attempt to drive yourself to a hospital. Dial the emergency number (911) to be transferred to a hospital with a coronary unit for an immediate treatment to unblock a coronary artery: thrombolysis and cardiac catheterization.
- Oxygen: It may be the first measure taken in the hospital or ambulance.
- Analgesics (pain management medications) such as morphine may be given if chest pain persists and is unbearable.
- Thrombolytics, such as streptokinase or a "tissue plasminogen activator," are medicines that dissolve clots that prevent blood flow. They can be administered either intravenously or directly into the clot through a catheter (a thin and flexible tube).
- Nitrates. Derivatives of nitroglycerin decrease the heart's work and oxygen needs They are usually taken in pills under the tongue or in a spray for angina pectoris. In the acute phase of a heart attack, they are usually used intravenously.
- Beta blockers. They work by blocking many of the effects of adrenaline in the body, which slows the heart rate and reduces its force. This means the heart requires less oxygen, and they also lower blood pressure.
- Digital. Drugs derived from digitalis, such as digoxin, stimulate the heart to pump more blood, which is useful if the heart attack causes heart failure.
- Calcium channel blockers prevent calcium from entering myocardial cells, which reduces the coronary arteries' tendency to narrow and the heart's oxygen needs. They also lower blood pressure. They are not usually used in the acute phase of a heart attack but may be used immediately after.
Bibliography
- Harrison’s, Principles of Internal medicine, 20th Edition (2018). Chapter 235: Electrocardiography. Pág. 4209. McGRAW-HILL EDUCATION. ISBN: 978-1259644030.
- First Aid for the Basic Sciences: Organ Systems (3rd Ed) 2017, Tao Le, William L. Hwang, Vinayak Muralidhar, Jared A. White and M. Scott Moore, ISBN: 978-1-25-958704-7, Pag. 87.
- Robbins Basic Pathology (10th Ed) 2018, Vinay Kumar, Abul K. Abbas, Jon C. Aster, ISBN: 978-0-323-35317-5, Pag. 411.
Show more
Rating Overview
Share your thoughts about this content